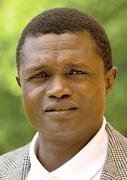





A travers ce texte, c’est avant tout l’humaniste et le chercheur ouvert aux sciences humaines que nous souhaitons remercier et auquel nous voulons rendre hommage.
Le Professeur Ogobara Doumbo avait compris l’intérêt des sciences humaines, comme outil au service de la santé publique. Il avait compris la nécessité d’une approche plus holistique des problèmes de santé et de pauvreté en Afrique et dans le monde. Il avait également compris que les sciences médicales et les sciences humaines devaient s’alimenter réciproquement pour prendre tout leur sens et atteindre leur objectif ultime: l’amélioration du bien-être des populations. Il avait compris ces aspects fondamentaux de l’interdisciplinarité sans arrière-pensée et dans un engagement altruiste total.
Certains d’entre nous à la FERDI, au CERDI au Centre d’économie de la Sorbonne ont été ses collègues et ses amis. D’autres ont également été ses élèves accueillis au MRTC - son centre de recherche et de formation sur le paludisme - comme tant d’étudiants africains, européens, asiatiques ou américains. Au total, ceux qui l’ont connu ont été les trois à la fois et sont unanimes sur le caractère avant-gardiste de son action, son humanisme, sa bienveillance et son humilité.
Certains ont dit que le Mali avait perdu son Victor Hugo de la recherche. Le Professeur était aussi un savant mélange de Louis Pasteur, d’Albert Schweitzer et de Hamadou Hampaté Bâ, s’il fallait se référer à quelques figures du passé pour souligner l’exception.
Mais le Professeur Ogobara Doumbo était avant tout un homme singulier au service d'autres hommes, tourné vers l’excellence de la recherche mais aussi vers l'action dans l’une des régions les plus pauvres et les plus instables du monde à ce jour. Co – fondateur de SANTE SUD, promoteur de la médecine de campagne au Mali et de la médecine générale communautaire, il a œuvré de façon concrète et pratique à établir non seulement un réseau de recherche de pointe mais également à lutter contre l’exclusion dans des régions reculées et extrêmement pauvres. Directeur du MRTC, directeur adjoint chargé du Pôle Mali de l’Unité mixte du CNRS « Environnement Santé et Société » et associé à d’autres centres de recherche en France et aux Etats-Unis (l’UMR SESSTIM, la Tulane School of Public Health), il a créé un modèle de développement par la recherche s’adossant à de nombreuses collaborations internationales et interdisciplinaires.
Un hommage issu du monde de la santé publique a été fait ici par des collègues qui appréciaient comme nous les valeurs du Professeur Doumbo. Nous retiendrons ici en complément quelques-unes de ses réalisations en lien avec les sciences humaines. A défaut de pouvoir mettre des mots sur l’immense vide laissé par le Professeur, nous avons voulu lister quelques publications dans ce domaine, pour que son œuvre serve d’exemple aux générations futures. Elles pourront trouver ici certaines de ses contributions scientifiques et s’en servir comme source d’inspiration.